0% found this document useful (0 votes)
71 views8 pagesHormonal Control of Calcium Homeostasis Chapter 9
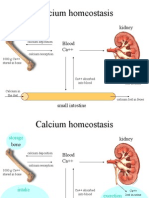
This document summarizes the hormonal control of calcium homeostasis. It discusses the roles of parathyroid hormone (PTH), vitamin D (calcitriol), and calcitonin in maintaining calcium levels. PTH increases calcium levels by promoting bone resorption and renal reabsorption of calcium. Vitamin D increases intestinal calcium absorption. Both PTH and vitamin D are regulated by calcium levels in a negative feedback loop. Calcium homeostasis requires tight regulation by these hormones to maintain appropriate calcium concentrations in the extracellular fluid and bones.
Uploaded by
Roua SafwatCopyright
© Attribution Non-Commercial (BY-NC)
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
71 views8 pagesHormonal Control of Calcium Homeostasis Chapter 9
This document summarizes the hormonal control of calcium homeostasis. It discusses the roles of parathyroid hormone (PTH), vitamin D (calcitriol), and calcitonin in maintaining calcium levels. PTH increases calcium levels by promoting bone resorption and renal reabsorption of calcium. Vitamin D increases intestinal calcium absorption. Both PTH and vitamin D are regulated by calcium levels in a negative feedback loop. Calcium homeostasis requires tight regulation by these hormones to maintain appropriate calcium concentrations in the extracellular fluid and bones.
Uploaded by
Roua SafwatCopyright
© Attribution Non-Commercial (BY-NC)
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
/ 8