0% found this document useful (0 votes)
98 views3 pagesNursing Diagnosis Interventions: Diarrhea Related To
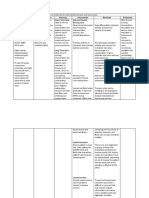
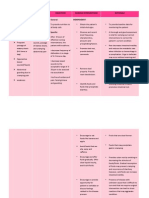
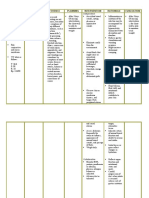
This document provides possible nursing diagnoses and interventions for gastrointestinal disorders. It lists diarrhea, risk for deficient fluid volume, anxiety, acute pain, and ineffective coping as potential nursing diagnoses. For each diagnosis, it outlines assessments and interventions such as monitoring intake and output, providing comfort measures, ensuring proper nutrition, and helping the patient develop effective coping strategies. The goal is to address factors causing the diagnoses and support the patient's physical and emotional needs.
Uploaded by
Editha Marie FloresCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
98 views3 pagesNursing Diagnosis Interventions: Diarrhea Related To
This document provides possible nursing diagnoses and interventions for gastrointestinal disorders. It lists diarrhea, risk for deficient fluid volume, anxiety, acute pain, and ineffective coping as potential nursing diagnoses. For each diagnosis, it outlines assessments and interventions such as monitoring intake and output, providing comfort measures, ensuring proper nutrition, and helping the patient develop effective coping strategies. The goal is to address factors causing the diagnoses and support the patient's physical and emotional needs.
Uploaded by
Editha Marie FloresCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
/ 3