ANATOMY AND PHYSIOLOGY
TOPIC:THE URINARY SYSTEM
REFERENCE: ESSENTIAL OF HUMAN ANATOMY (EIGHT EDITION) BY ELAINE MARIEB
PROFESSOR: MA. ROSARIO MEÑEZ-QUEJADO, RMT, Ed.D.
Functions of the Urinary System
Elimination of waste products
Nitrogenous wastes, Toxins, Drugs
Regulate aspects of homeostasis
Water balance
Electrolytes
Acid-base balance in the blood
Blood pressure
Red blood cell production
Activation of vitamin D
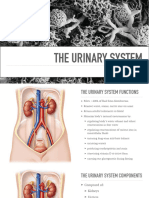
Organs of the Urinary system
Kidneys
Ureters
Urinary bladder
Urethra
Location of the Kidneys
Against the dorsal body wall
At the level of T12 to L3
The right kidney is slightly lower than the left
Attached to ureters, renal blood vessels, and nerves at renal hilus
Atop each kidney is an adrenal gland
Coverings of the Kidneys
Renal capsule
Surrounds each kidney
Adipose capsule
Surrounds the kidney
Provides protection to the kidney
Helps keep the kidney in its correct location
Regions of the Kidney
Renal cortex – outer region
Renal medulla – inside the cortex
Renal pelvis – inner collecting tube
Kidney Structures
Medullary pyramids – triangular regions of tissue in the medulla
Renal columns – extensions of cortex-like material inward
Calyces – cup-shaped structures that funnel urine towards the renal pelvis
Blood Flow in the Kidneys
Nephrons
The structural and functional units of the kidneys
Responsible for forming urine
Main structures of the nephrons
Glomerulus
Renal tubule
Glomerulus
A specialized capillary bed
Attached to arterioles on both sides (maintains high pressure)
Large afferent arteriole
� Narrow efferent arteriole
Capillaries are covered with podocytes from the renal tubule
The glomerulus sits within a glomerular capsule (the first part of the renal tubule)
Renal Tubule
Glomerular (Bowman’s) capsule
Proximal convoluted tubule
Loop of Henle
Distal convoluted tubule
Types of Nephrons
Cortical nephrons
Located entirely in the cortex
Includes most nephrons
Juxtamedullary nephrons
Found at the boundary of the cortex and medulla
Peritubular Capillaries
Arise from efferent arteriole of the glomerulus
Normal, low pressure capillaries
Attached to a venule
Cling close to the renal tubule
Reabsorb (reclaim) some substances from collecting tubes
Urine Formation Processes
Filtration
Reabsorption
Secretion
Filtration
Nonselective passive process
Water and solutes smaller than proteins are forced through capillary walls
Blood cells cannot pass out to the capillaries
Filtrate is collected in the glomerular capsule and leaves via the renal tubule
Reabsorption
The peritubular capillaries reabsorb several materials (Some water, Glucose
Amino acids, Ions)
Some reabsorption is passive, most is active
Most reabsorption occurs in the proximal convoluted tubule
Materials Not Reabsorbed
Nitrogenous waste products (Urea, Uric acid, Creatinine) and Excess water
Secretion – Reabsorption in Reverse
Some materials move from the peritubular capillaries into the renal tubules
(Hydrogen and potassium ions , Creatinine)
Materials left in the renal tubule move toward the ureter
Formation of Urine
Characteristics of Urine Used for Medical Diagnosis
Colored somewhat yellow due to the pigment urochrome (from the destruction of hemoglobin) and
solutes
Sterile
Slightly aromatic
Normal pH of around 6
Specific gravity of 1.001 to 1.035
Ureters
Slender tubes attaching the kidney to the bladder
Continuous with the renal pelvis
Enter the posterior aspect of the bladder
Runs behind the peritoneum
� Peristalsis aids gravity in urine transport
Urinary Bladder
Smooth, collapsible, muscular sac
Temporarily stores urine
Trigone – three openings (Two from the ureter and One to the urethra)
Urinary Bladder Wall
Three layers of smooth muscle (detrusor muscle)
Mucosa made of transitional epithelium
The Urinary System
Walls are thick and folded in an empty bladder
Bladder can expand significantly without increasing internal pressure
Urethra
Thin-walled tube that carries urine from the bladder to the outside of the body by peristalsis
Release of urine is controlled by two sphincters
Internal urethral sphincter (involuntary)
External urethral sphincter (voluntary)
Urethra Gender Differences
Length
Females – 3–4 cm (1 inch) Males – 20 cm (8 inches)
Location
Females – along wall of the vagina Males – through the prostate and penis
Function
Females – only carries urine
Males – carries urine and is a passageway for sperm cells
Micturition (Voiding)
Both sphincter muscles must open to allow voiding
The internal urethral sphincter is relaxed after stretching of the bladder
Activation is from an impulse sent to the spinal cord and then back via the pelvic splanchnic
nerves
The external urethral sphincter must be voluntarily relaxed
Maintaining Water Balance
Normal amount of water in the human body
Young adult females – 50%
Young adult males – 60%
Babies – 75%
Old age – 45%
Water is necessary for many body functions and levels must be maintained
Distribution of Body Fluid
Intracellular fluid (inside cells)
Extracellular fluid (outside cells)
Interstitial fluid
Blood plasma
The Link Between Water and Salt
Changes in electrolyte balance causes water to move from one compartment to another
Alters blood volume and blood pressure
Can impair the activity of cells
Maintaining Water Balance
Water intake must equal water output
Sources for water intake
Ingested foods and fluids
Water produced from metabolic processes
Sources for water output
Vaporization out of the lungs
� Lost in perspiration
Leaves the body in the feces
Urine production
Dilute urine is produced if water intake is excessive
Less urine (concentrated) is produced if large amounts of water are lost
Proper concentrations of various electrolytes must be present
Regulation of Water and Electrolyte Reabsorption
Regulation is primarily by hormones
Antidiuretic hormone (ADH) prevents excessive water loss in urine
Aldosterone regulates sodium ion content of extracellular fluid
Triggered by the rennin-angiotensin mechanism
Cells in the kidneys and hypothalamus are active monitors
Maintaining Water and Electrolyte Balance
Maintaining Acid-Base Balance in Blood
Blood pH must remain between 7.35 and 7.45 to maintain homeostasis
Alkalosis – pH above 7.45
Acidosis – pH below 7.35
Most ions originate as byproducts of cellular metabolism
Most acid-base balance is maintained by the kidneys
Other acid-base controlling systems
Blood buffers
Respiration
Blood Buffers
Molecules react to prevent dramatic changes in hydrogen ion (H+) concentrations
Bind to H+ when pH drops
Release H+ when pH rises
Three major chemical buffer systems
Bicarbonate buffer system
Phosphate buffer system
Protein buffer system
The Bicarbonate Buffer System
Mixture of carbonic acid (H2CO3) and sodium bicarbonate (NaHCO3)
Bicarbonate ions (HCO3–) react with strong acids to change them to weak acids
Carbonic acid dissociates in the presence of a strong base to form a weak base and water
Respiratory System Controls of Acid-Base Balance
Carbon dioxide in the blood is converted to bicarbonate ion and transported in the plasma
Increases in hydrogen ion concentration produces more carbonic acid
Excess hydrogen ion can be blown off with the release of carbon dioxide from the lungs
Respiratory rate can rise and fall depending on changing blood pH
Renal Mechanisms of Acid-Base Balance
Excrete bicarbonate ions if needed
Conserve or generate new bicarbonate ions if needed
Urine pH varies from 4.5 to 8.0
Developmental Aspects of the Urinary System
Functional kidneys are developed by the third month
Urinary system of a newborn
Bladder is small
Urine cannot be concentrate
Control of the voluntary urethral sphincter does not start until age 18 months
Urinary infections are the only common problems before old age
Aging and the Urinary System
There is a progressive decline in urinary function
The bladder shrinks with aging
� Urinary retention is common in males