0% found this document useful (0 votes)
38 views7 pagesIMCI
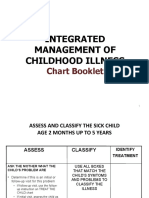
The Integrated Management of Childhood Illness (IMCI) is a strategy aimed at reducing mortality and morbidity in children under five by addressing major communicable diseases through both preventive and curative measures. The goal is to reduce infant and under-five mortality rates by one third by 2010 and by two thirds by 2015, with a focus on improving case management skills of health workers and family practices. Key components include assessing symptoms, classifying illnesses, and providing appropriate treatments for conditions such as pneumonia, diarrhea, and malaria.
Uploaded by
talentoashlee07Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
38 views7 pagesIMCI
The Integrated Management of Childhood Illness (IMCI) is a strategy aimed at reducing mortality and morbidity in children under five by addressing major communicable diseases through both preventive and curative measures. The goal is to reduce infant and under-five mortality rates by one third by 2010 and by two thirds by 2015, with a focus on improving case management skills of health workers and family practices. Key components include assessing symptoms, classifying illnesses, and providing appropriate treatments for conditions such as pneumonia, diarrhea, and malaria.
Uploaded by
talentoashlee07Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
/ 7