0% found this document useful (0 votes)
85 views71 pagesNursing Ethics & Legal Concepts
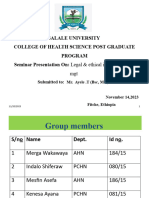
The document outlines the learning objectives related to ethics and legal concepts in nursing, including definitions, types of ethics, and ethical theories. It also discusses the legal framework governing nursing practice, including types of law, legal actions, and common legal issues in Ethiopia, particularly regarding abortion. Additionally, it addresses ethical dilemmas and decision-making processes in nursing, emphasizing the importance of patient preferences and contextual factors.
Uploaded by
Mila RetaCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPT, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
85 views71 pagesNursing Ethics & Legal Concepts
The document outlines the learning objectives related to ethics and legal concepts in nursing, including definitions, types of ethics, and ethical theories. It also discusses the legal framework governing nursing practice, including types of law, legal actions, and common legal issues in Ethiopia, particularly regarding abortion. Additionally, it addresses ethical dilemmas and decision-making processes in nursing, emphasizing the importance of patient preferences and contextual factors.
Uploaded by
Mila RetaCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPT, PDF, TXT or read online on Scribd
/ 71