25
Journal of Pediatric Intensive Care 1 (2012) 2529
DOI 10.3233/PIC-2012-005
IOS Press
Nurse staffing levels on the NPICU
in the island of Malta
Victor Grech*, Maria Cassar and Sandra Distefano
Paediatric Department, Mater Dei Hospital, Malta
Abstract
Purpose. Nurse staffing levels in neonatal paediatric intensive care units (NPICU) are often inadequate. Malta is a small Island in
the centre of the Mediterranean (total population around 400,000) with a birth rate of just under 4000/annum, with one NPICU.
This study analysed nurse staffing levels for a 1 year period in order to ascertain whether said levels are adequate or not.
Methods. Daily ward occupancies were classified by level of dependency, and ideal nursing requirements were estimated using
internationally approved standards, on a daily basis, for the period 12 month period from 01/04/2008 to 31/03/2009. These were
compared with the actual daily morning nursing levels to estimate deficit/s.
Results. There were a total of 373 admissions to the unit resulting in a total of 5464 patient days (daily census at 0700 hrs) and 1471
free bed days (occupancy 78.8%). Occupancy varied between 8 and 23 patients (mean 15). Staffing levels ranged between 7 and 17
nurses (mean 11). The overall mean deficit was of 3.3 nurses, but this ranged from a maximum of 11 to a rare surplus of 7 nurses.
Conclusions. This study only focused on a daily morning snapshot where the nursing staff is at its peak number the nocturnal
deficit is naturally worse. Furthermore, experience levels vary due to short rotations through the unit of inexperienced midwifery
staff. Moreover, there are no staff designated as responsible for further education and training, extra staff for unpredictable high
dependency situations, to compensate for leave, sickness, maternity leave, study leave, staff training and attendance at meetings.
Clearly, the Maltese NPICU is overall understaffed.
Keywords: Hospital bed capacity/statistics & numerical data, humans, infant, newborn, intensive care units, neonatal/manpower/
*statistics & numerical data, personnel staffing and scheduling/statistics & numerical data, workload/statistics & numerical
data
Introduction
The best quality neonatal care possible is crucial for
the outcome of sick neonates as this minimises
morbidity and mortality [1]. A reduction in morbidity
will inevitably also reduce the long-term burden of care
on the state [2]. It has been shown that throughout
Europe, since the 1990s, with increasing utilization of
surfactant and antenatal steroid administration for anticipated premature deliveries (and higher survival rates of
such neonates), there has been an increased requirement
for neonatal intensive cot utilization. Such cots are
low-volume and high cost, and are required at a level
of 1.01.9 cots per 1000 population with an average
*Corresponding author: Victor Grech, Paediatric Dept., Mater Dei
Hospital, Malta. Tel.: +356 99495813, E-mail: victor.e.grech@gov.mt.
70% occupancy [1]. It has been estimated that 12
neonates per 100 live births require at least 1 hour of
intensive care [3].
It has been shown that for these neonates, the risk
adjusted mortality rises linearly with level of occupancy,
such that infants admitted to full units have 50% greater
odds of dying than those admitted to units which are
only half full [3]. It is clearly crucial that staff levels
are appropriate to the dependency of the neonates, that
is, to the recommended nurse to patient ratios depending
on the severity of the condition being treated, as will be
explained below [1]. For this reason, it is recommended
that neonatal units should be planned to have an average
occupancy of 70% [1]. Malta has strong links with
the United Kingdom, with almost all trainees visiting
the United Kingdon. Systems in place therefore are virtually identical to the British system. The staffing
2146-4618/12/$27.50 2012 IOS Press and the authors. All rights reserved
�26
V. Grech et al. / Nurse staffing levels on the NPICU in the island of Malta
recommendations that are used in this study (see below)
are those used in the UK. These recommendations
remain in use although they are based on studies performed in the early 1990s, and must therefore be
regarded as minimum standards [4,5].
The level of dependency is determined by the acuity
and severity of the neonates condition/s, and the
greater the acuity and severity, the greater the recommended nurse to patient ratio will be [1].
Neonates in intensive care situations should have 1:1
nursing, and critically ill neonates (e.g. severe pulmonary hypertension) should have 2 nurses in attendance [6].
High dependency and special care should have
nurse to baby ratios of at least 1:2 and 1:4 respectively
[1]. Inclusion criteria for the various categories are
shown in table 1.
Setting
The Maltese Neonatal Paediatric Intensive Care Unit
(NPICU formerly St. Lukes Hospital Special Care
Baby Unit) is the only unit serving the Maltese
Table 1
Inclusion criteria for babies on the neonatal paediatric intensive care
unit
Intensive Care
Intubated and 1st 24 hours extubated.
NCPAP (nasal continuous positive airway pressure) at all and
<5 days old.
NCPAP at all and <1000g and for 24 hours after removal.
<29 weeks of gestation and <48 hours old.
Requiring major emergency surgery preoperatively and 24 hrs
postoperatively.
Complex procedures: Full exchange procedures, peritoneal
dialysis, infusion of inotrope or pulmonary vasodilator or
prostaglandin and for 24 hours after.
On day of death.
Other very unstable situations.
High Dependency
NCPAP and not filling any of the above criteria for
intensive care.
<1000g and not filling any of the above criteria for
intensive care.
Parenteral nutrition.
Fits.
Oxygen therapy and < 1500g.
Neonatal abstinence syndrome.
Complex procedures not as above: Partial exchange, arterial
line, chest drain, tracheostomy.
Severe apnoeas requiring recurrent stimulation.
Special Care
Any other condition not reasonably expected to be looked after
at home.
Archipelago, with a total catchment area of approximately 400,000 population and a live birth rate of just
under 4000 per annum [7]. The NPICU is a Level 3
Unit providing the whole range of medical neonatal
care. A Level 3 unit provides the whole range of medical neonatal care but not necessarily all specialist services such as neonatal surgery. Continuing neonatal
intensive care is also provided and is staffed by consultants whose principal duties are to the unit. There is 24hour resident cover by Higher Specialist Trainee in
paediatrics who has worked a minimum of four months
in neonatology. This doctor is available for the unit at
all times and is not required to cover any other service.
Two of the authors work on the unit, one as the
Nursing Officer in charge of the unit and the other as
the paediatric cardiologist for the country.
The unit officially has a total maximum capacity of 19
patients but this figure is not absolute in that since there
are no other units in the country, the unit stretches to
accommodate whatever number of admissions are
needed. The medical staff consists of three consultants
and two resident specialists, assisted by two basic specialist trainees. The on-call medical staff consists of a consultant covering the unit with two resident specialists on-site.
The nursing staff works on a 12 hour shift starting
and ending at 0700 hours and 1900 hours respectively
(day, night, rest and off) and each shift comprises 7 to
8 individuals. In addition, there are 4 to 5 nurses who
work daytime hours, i.e. up to 1600 to 1900 hours.
These figures do not include 2 unit nurses who manage the ward and also help out with general nursing
care if the need arises. In our unit, vacation leave is
only allowed for 1 member of rota staff and 1 member
of day staff.
During the period under study, the nursing staff
consisted of 39 full-time equivalents, with 45 individual nurses in total. There are a total of four shifts
with no nominated educators.
For the purposes of patient safety, these nurses or
midwives work completely supervised for the first
3 months of their rotation. Staff who work unsupervised
therefore have a minimum of 3 months of experience.
The level of individual experience varies from years to
decades.
The case mix is similar, year by year, and for the last
available year, admissions by gestational age were as
follows: 3 under 25 weeks of gestation, 14 between 25
and 27 weeks, 38 between 31 and 33 weeks, 64 between
34 and 36 weeks. There were also a total of 136 term
admissions and 44 paediatric admissions. Parent education is ad hoc and done by unit nurses.
�V. Grech et al. / Nurse staffing levels on the NPICU in the island of Malta
This study analyses admission data to the Maltese
NPICU for the period 01/04/200831/03/2009, and
compares unit patient occupancy with nurse staffing
levels on a daily basis. This was done in order to estimate daily deficits (if any) of nurse staffing levels in
relation to daily patient occupancy, after stratifying
patients to level of acuity in order to determine the individual level of ideal nurse to patient ratio, and total ideal
number of nurses that would have been needed on each
and every day. This was compared with the actual number of staff present, on each day, in order to identify days
where any staff deficits were definitely present.
Methods
Daily ward occupancies were compiled in an Excel
spreadsheet, and patients were classified as per table 1
as per recommended guidelines, [1] by the Nursing Officer in charge of the unit, on a daily basis, as a morning
snapshot. Morning nursing levels were also documented.
The data was entered into Excel by the ward clerk, on a
daily basis, and entry was checked by both authors.
Ideal daily nursing requirements were estimated
based on the above daily number of patients and their
dependency as per guidelines by diagnosis (table 1) [1]
i.e. patients requiring critical care should have 2 staff
in attendance, patients requiring intensive care should
require 1:1 nursing, patients requiring high dependency
and special care should have nurse to baby ratios of at
least 1:2 and 1:4 respectively [1]. The daily morning
nursing excess/deficit could therefore be calculated by
subtracting the desired number of nurses from the actual
number of nurses present as per above calculation.
The most severe condition requiring the greatest
level of dependency was utilized in patients with multiple diagnoses.
Official hospital admission and occupancy statistics
for NPICU for the period under study were also obtained.
Ethical approval was not sought as no patients/parents
were contacted and data was anonymised.
Results
There were a total of 373 admissions to the unit for
the period 01/04/200831/03/2009. These produced a
total of 5464 patient days (daily census at 0700 hrs).
Cot days by diagnosis are shown in table 2. Based on
an official estimate of a total maximum unit capacity
of 19 patients, there were 1471 free bed days with a total
27
bed occupancy of 78.8%. The average length of stay
was 14.6 days. There were a total of 38 non-neonatal
patients, with an age up to 3 years.
Summary statistics are given in table 3. Unit occupancy varied widely, and never fell below 8 patients,
and the maximum occupancy was 23 (mean 15). Staffing levels were equally variable, ranging between
7 and 17 nurses (mean 11). The overall mean deficit
was of 3.3 nurses, but this ranged from a maximum
of 11 to a surplus of 7 nurses. The deficits were unrelated to weekends, holiday periods or season.
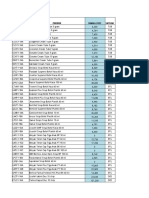
The trend in nursing deficit (and occasional surplus)
is depicted as a histogram in (Fig. 1). Values above the
baseline are nursing staff deficits, while values below
the baseline are nursing staff surpluses.
Discussion
Our study calculates desired daily staffing levels by
assigning individual daily patient dependency according
to the individual patient diagnosis, using published
Table 2
Cot days by diagnosis using table 1
Intensive Care
Intubated and 1st 24 hours extubated.
NCPAP (nasal continuous positive airway pressure)
at all and <5 days old.
NCPAP at all and <1000g and for 24 hours after
removal.
<29 weeks of gestation and <48 hours old.
Requiring major emergency surgery preoperatively and
24 hrs postoperatively.
Complex procedures: Full exchange procedures,
peritoneal dialysis, infusion of inotrope or
pulmonary vasodilator or prostaglandin and for 24
hours after.
On day of death.
Other very unstable situations.
High Dependency
NCPAP and not filling any of the above criteria for
intensive care.
<1000g and not filling any of the above criteria for
intensive care.
Parenteral nutrition.
Fits.
Oxygen therapy and < 1500g.
Neonatal abstinence syndrome.
Complex procedures not as above: Partial exchange,
arterial line, chest drain, tracheostomy.
Severe apnoeas requiring recurrent stimulation.
Special Care
Any other condition not reasonably expected to be
looked after at home.
Total
564
900
14
19
85
68
2
2806
0
0
0
4
28
208
12
0
536
5464
�28
V. Grech et al. / Nurse staffing levels on the NPICU in the island of Malta
Table 3
Summary statistics for unit occupancy, staffing levels, and staffing deficit for the entire period under study: 01/04/200831/03/2009
Mean
Standard Error
Median
Mode
Standard Deviation
Sample Variance
Minimum
Maximum
Unit occupancy
Nursing staff
Nursing deficit
15
0.14
15
17
2.6
7.0
8
23
11
0.09
11
11
1.7
3.0
7
17
3.3
0.17
4
4
3.2
10.4
7
11
recommendations, [1] and comparing the total derived
daily ideal nursing complement with the actual nursing
complement on that same day. This study shows an
overall deficit in the ideal level of staffing, except for a
few weeks toward the end of the study wherein the
admission rate temporarily fell.
Our study is limited by the fact that it only takes into
account one single unit, that is, the only such unit available in the country. This paper also focused on a daily
morning snapshot where the nursing staff is at its peak
number, and it is clear that the nocturnal deficit is therefore worse due to the absence of additional day only
staff. Indeed, the night shift consists, on average, of
78 nursing staff. This study also could not take into
consideration nursing experience levels as the staffing
is usually a mixture of variably experienced nurses and
midwives. For example, for the first 6 months of this
study (up to November 2008), a group of 6 midwives
were completing a 1 year rotation in NPICU. The subsequent rotation comprised 5 midwives, only 2 of which
were assigned to NPICU for a year, while the other
3 were only assigned for 6 months. For the purposes
of patient safety, these midwives work completely
supervised for the first 3 months of their rotation, hence
their addition to the dataset as full members of staff
is misleading. This rotation includes obstetric and
gynaecology wards, antenatal clinics, antenatal ultrasound and labour ward, hence little experience or preparation is gained preparatory to a tour of work on
NPICU.
In addition, the following paramedical staff does not
exist in our unit but is also recommended: a designated
nurse responsible for further education and training,
extra staff for unpredictable situations, e.g. one nurse
11
9
7
3
1
01
/0
4
15 /08
/0
4
29 /08
/0
4
13 /08
/0
5
27 /08
/0
5
10 /08
/0
6
24 /08
/0
6
08 /08
/0
7
22 /08
/0
7
06 /08
/0
8
19 /08
/0
8
02 /08
/0
9
16 /08
/0
9
30 /08
/0
9
14 /08
/1
0
28 /08
/1
0
11 /08
/1
1
25 /08
/1
1
09 /08
/1
2
23 /08
/1
2
06 /08
/0
1
20 /09
/0
1
03 /09
/0
2
17 /09
/0
2
03 /09
/0
3
17 /09
/0
3
31 /09
/0
3/
09
Deficit
3
5
7
Date
Fig. 1. Nursing staff deficit over the period 01/04/2008-31/03/2009.
�V. Grech et al. / Nurse staffing levels on the NPICU in the island of Malta
available on each shift for intensive or high dependency
cover, and extra staff to compensate for leave, sickness,
maternity leave, study leave, staff training and attendance at meetings [1]. This recommendation does not
include administration and secretarial cover.
Nursing deficits are common worldwide, and such
deficits, in themselves, may contribute to burnout,
reduced quality of care and carers actually opting out of
their profession [8]. Indeed, quality of care may deteriorate to levels such that unmet nursing care needs directly
lead to adverse events, up to and including death [9].
A nursing deficit is not uncommon in neonatal units,
and in the UK, it has been estimated that 79% of neonatal intensive care units have such deficits [1012].
One may speculate that this may be due not only to a
general lack of nursing cover, but also to the stress that
these jobs engender in staff, making them unpalatable
to employees in the long term. It has also been suggested that the increasing pressure to reduce the working hours all medical and paramedical staff and the
increasing duration of neonatal nurse training inevitably makes it more difficult for units to maintain staff
skills and to prioritise training [12,13].
It has been unequivocally shown that risk-adjusted
mortality in very low birthweight or preterm infants is
associated with levels of nursing provision. For example, increasing the ratio of experienced nurses is associated with a decrease in risk-adjusted mortality [14].
Increasing the total ratio of nurse to patient has also been
shown to significantly reduce mortality on neonatal units
[14]. Indeed, staffing variations across units within the
same country (Canada) have also been shown to affect
outcome [15]. Staffing levels appear to be such a contentious issue that some researchers have also suggested
ways in which safer staffing of neonatal units may
achieved, including network-wide workforces, clinical
support workers and neonatal housekeepers [12].
Conclusion
As measured against the quoted recommended
staffing levels, the NPICU has often been understaffed during the period under study as measured
by the data and methods used, albeit the situation
29
appears to have temporarily improved toward the
study period. We hope that this analysis will prompt
the local Health Authorities to assign a higher priority
to staffing levels in our unit.
References
[1] British Association of Perinatal Medicine. Standards for hospitals providing neonatal intensive and high dependency care.
London: BAPM; 1996.
[2] Hack M. Consideration of the use of health status, functional
outcome, and quality-of-life to monitor neonatal intensive
care practice. Pediatrics 1999; 103: 31928.
[3] International Neonatal Network, Scottish Neonatal Consultants, Nurses Collaborative Study Group. Risk adjusted and
population based studies of the outcome for high risk infants
in Scotland and Australia. Arch Dis Child Fetal Neonatal Ed
2000; 82: F11823.
[4] Williams S, Whelan A, Weindling AM, Cooke RWI. Nursing
requirements for neonatal intensive care. Arch Dis Child
1993; 68: 5348.
[5] Northern Neonatal Network. Measuring neonatal nursing
workload. Arch Dis Child 1993; 68: 53943.
[6] Standards for Paediatric Intensive Care. London: Paediatric
Intensive Care Society; 1996.
[7] National Statistics Office. National Statistics Office, Malta:
Demographic Review for the Maltese Islands (annual publication); 2008.
[8] Poghosyan L, Clarke SP, Finlayson M, Aiken LH. Nurse
burnout and quality of care: cross-national investigation in
six countries. Res Nurs Health 2010; 33: 28898.
[9] Lucero RJ, Lake ET, Aiken LH. Nursing care quality and
adverse events in US hospitals. J Clin Nurs 2010; 19: 218595.
[10] Tucker J, Tarnow-Mordi W, Gould C, Parry G, Marlow N.
UK neonatal intensive care services in 1996. On behalf of
the UK Neonatal Staffing Study Collaborative Group. Arch
Dis Child Fetal Neonatal Ed 1999; 80: F2334.
[11] Tucker J. UK Neonatal Staffing Study Group. Patient volume,
staffing, and workload in relation to risk-adjusted outcomes in
a random stratified sample of UK neonatal intensive care
units: a prospective evaluation. Lancet 2002; 359: 99107.
[12] Watkin SL. Managing safe staffing. Semin Fetal Neonatal
Med 2005; 10: 918.
[13] Hamilton KE, Redshaw ME, Tarnow-Mordi W. Nurse staffing in relation to risk-adjusted mortality in neonatal care.
Arch Dis Child Fetal Neonatal Ed 2007; 92: F99103.
[14] Callaghan LA, Cartwright DW, ORourke P, Davies MW.
Infant to staff ratios and risk of mortality in very low birthweight
infants. Arch Dis Child Fetal Neonatal Ed 2003; 88: F947.
[15] Lee SK, McMillan DD, Ohlsson A, Pendray M, Synnes A,
Whyte R, Chien LY, Sale J. Variations in practice and outcomes in the Canadian NICU network: 19961997. Pediatrics 2000; 106: 10709.