100% found this document useful (12 votes)
9K views2 pagesSleep Disorder Evaluation Template
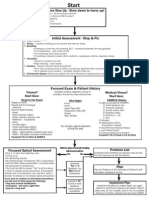
The Sleep Disorder evaluation MedicalTemplate is suitable for any physician or health care provider that evaluates patients with sleep disorders such as sleep apnea, narcolepsy, or restless leg syndrome.
Sleep disorders include obstructive sleep apnea, narcolepsy, restless leg syndrome, insomnia, night terrors and others. The National Center on Sleep Disorders Research (NCSDR) estimates that 42 million Americans suffer from a chronic sleep disorder. Sleep disorders are associated with chronic sleep deprivation, elevated blood pressure, cardiovascular disease, pulmonary hypertension, cognitive dysfunction, erectile dysfunction, chronic fatigue, and other medical conditions that result in $15.9 billion in health care costs annually. Sleep disorders can have a detrimental influence in the workplace and school performance, and people who are chronically sleep deprived due to sleep disorders are at increased risk of auto accidents.
The Sleep Disorder Evaluation MedicalTemplate has prompters for the sleep history, medical history, medication use that affects sleep architecture, drug use history, auto accident history, physical examination, and testing options. This assists physicians in efficiently documenting a thorough history.
Uploaded by
e-MedToolsCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
100% found this document useful (12 votes)
9K views2 pagesSleep Disorder Evaluation Template
The Sleep Disorder evaluation MedicalTemplate is suitable for any physician or health care provider that evaluates patients with sleep disorders such as sleep apnea, narcolepsy, or restless leg syndrome.
Sleep disorders include obstructive sleep apnea, narcolepsy, restless leg syndrome, insomnia, night terrors and others. The National Center on Sleep Disorders Research (NCSDR) estimates that 42 million Americans suffer from a chronic sleep disorder. Sleep disorders are associated with chronic sleep deprivation, elevated blood pressure, cardiovascular disease, pulmonary hypertension, cognitive dysfunction, erectile dysfunction, chronic fatigue, and other medical conditions that result in $15.9 billion in health care costs annually. Sleep disorders can have a detrimental influence in the workplace and school performance, and people who are chronically sleep deprived due to sleep disorders are at increased risk of auto accidents.
The Sleep Disorder Evaluation MedicalTemplate has prompters for the sleep history, medical history, medication use that affects sleep architecture, drug use history, auto accident history, physical examination, and testing options. This assists physicians in efficiently documenting a thorough history.
Uploaded by
e-MedToolsCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
/ 2