0% found this document useful (0 votes)
56 views22 pagesNotes
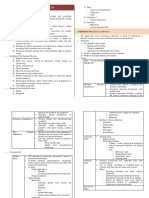
The document outlines the nursing process as a systematic, patient-centered approach consisting of five steps: assessment, diagnosis, planning, implementation, and evaluation. It emphasizes the importance of critical thinking, patient-centered care, and various frameworks like Maslow's Hierarchy of Needs and SBAR communication. Additionally, it covers essential nursing procedures, pharmacokinetics, pharmacodynamics, medication administration, and quality assurance in nursing care.
Uploaded by
Katrina Jhane MercadoCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
56 views22 pagesNotes
The document outlines the nursing process as a systematic, patient-centered approach consisting of five steps: assessment, diagnosis, planning, implementation, and evaluation. It emphasizes the importance of critical thinking, patient-centered care, and various frameworks like Maslow's Hierarchy of Needs and SBAR communication. Additionally, it covers essential nursing procedures, pharmacokinetics, pharmacodynamics, medication administration, and quality assurance in nursing care.
Uploaded by
Katrina Jhane MercadoCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
/ 22